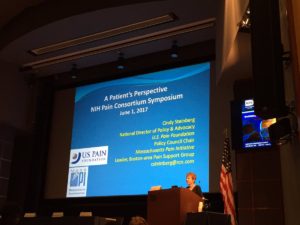
 U.S. Pain’s National Director of Policy and Advocacy, Cindy Steinberg, was invited to present the patient perspective at the National Institutes of Health (NIH) 12th Annual Pain Consortium Symposium on May 31 and June 1. Each year, noted researchers working in the field of pain management are invited to present their research findings and an award is given to a junior investigator who has done outstanding pain research.This year, the theme was, “Multidisciplinary Strategies for Pain Management.”
U.S. Pain’s National Director of Policy and Advocacy, Cindy Steinberg, was invited to present the patient perspective at the National Institutes of Health (NIH) 12th Annual Pain Consortium Symposium on May 31 and June 1. Each year, noted researchers working in the field of pain management are invited to present their research findings and an award is given to a junior investigator who has done outstanding pain research.This year, the theme was, “Multidisciplinary Strategies for Pain Management.”
In her presentation, in addition to stressing the necessity of multimodal, integrated pain care, Steinberg said that the most successful pain management results when doctors partner with their patients to find treatments that work for them. Steinberg pointed out that, in most cases, chronic pain is a lifelong illness that requires long-term support. There will be ups and downs, relapses, improvements and set-backs, and it is key to find a well-run support group, understanding family and friends, or a trusted therapist.
Regarding research, Steinberg made a plea for more and better epidemiological data, analysis, and reporting on pain. She emphasized the lack of basic data on the incidence and prevalence of various pain conditions, on the health consequences of pain in terms of morbidity, disability and mortality, and on the cost of pain to our economy, in terms of utilization of medical services and indirect costs, such as missed work days and reductions in productivity is hindering progress in the field and perpetrating the lack of public awareness, professional education and research investment in chronic pain. Steinberg also called for a closer working relationship between pain researchers and people living with chronic pain whose experience of the disease as well as lessons learned could help inform future research.
Some highlights from noted researchers included Dr. Dennis Turk from the University of Washington reporting that using one therapy for pain management is at best only modestly successful and combinations of treatments are essential. For example, Turk stated that medications reduce pain by 30 percent to 40 percent in fewer than 50 percent of patients. Meanwhile, injections, which are the mostly commonly used treatment, show no evidence of positive short-term effects and their long-term effects are unknown.
Dr. Peggy Compton from the University of Pennsylvania spoke about managing complex cases of both substance use disorder (SUD) and chronic pain. She said that epidemiologically complex pain patients are not typically prescription opioid abusers, as those with SUD tend to be young (18-26 year olds) and male. Complex pain patients tend to be older (above 45 years old) and female. Compton also noted that the key improvement clinicians should look for with any treatment is improvement in function.
Dr. Robert Kerns, of the Veterans Health Administration, spoke about models of integrated pain care at Veterans Affairs (VA) and said that “integrated” does not have to be “co-located” as the VA has used distributed and virtual care successfully. He said that the goals of treatment, in addition to pain reduction, should include reduction in emotional distress, improved quality of life, and optimal functioning. The VA has modified their Step Care Model to include self-care as a key component of successful pain management.
The symposium was streamed live and the recording is available for viewing here.
