 On Sept. 24, the Alliance to Advance Comprehensive Integrative Pain Management (AACIPM) hosted a virtual symposium, “Equity in Access to Comprehensive Integrative Pain Management in Chronic Pain,” in partnership with the U.S. Pain Foundation. Throughout the day, patients, providers, policymakers, and payors shared information and ideas to help bridge the gap between quality pain care and underserved communities.
On Sept. 24, the Alliance to Advance Comprehensive Integrative Pain Management (AACIPM) hosted a virtual symposium, “Equity in Access to Comprehensive Integrative Pain Management in Chronic Pain,” in partnership with the U.S. Pain Foundation. Throughout the day, patients, providers, policymakers, and payors shared information and ideas to help bridge the gap between quality pain care and underserved communities.
U.S. Pain Foundation CEO Nicole Hemmenway spoke on the results of the organization’s August survey about barriers to multidisciplinary care, which received 1,581 responses.
“The findings from the survey align with what we, as an organization, hear every day from patients: although experts agree that the best pain care is multidisciplinary, multimodal, and individualized, patients don’t really have access to that type of care,” said Hemmenway in her remarks.
Hemmenway reviewed key takeaways from the survey, including:
- Most patients lack access to multidisciplinary and integrative pain care
- Cost is the biggest barrier to pain management
- Behavioral health and pain must be further addressed
- Accelerated access to telehealth has been a silver lining of pandemic
[su_pullquote align=”right”]To watch the day’s events or download the slides, visit AACIPM’s site.[/su_pullquote]
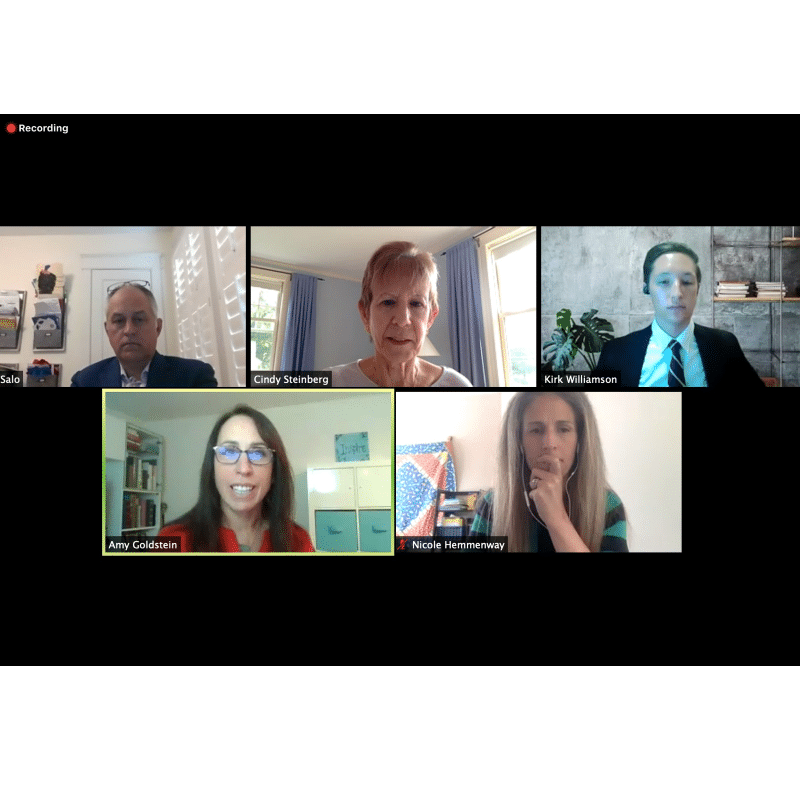
Later in the day, U.S. Pain’s National Policy Advisor Cindy Steinberg moderated a question and answer session featuring Hemmenway, United Health Venture’s David Elton, National Governors Association’s Kirk Williamson, and National Association of Medicaid Directors’s Matt Salo.
During the panel discussion, Steinberg asked all the panelists about the number one approach to increasing access to complementary pain care (meaning chiropractic, acupuncture, massage, yoga, and tai chi) for individuals living in underserved communities and the steps needed to implement these strategies. While all the panelists agreed on the importance of implementing such care, they said that the process is slow-moving and must be implemented on a trial basis in each state to determine the cost-benefit ratio before such strategies could be implemented federally.
“We were honored to be involved with this event, which was perfectly timed with Pain Awareness Month,” says Hemmenway. “Chronic pain is a challenging, complicated health condition; improving pain care is equally challenging and complicated. It’s vital to bring together diverse stakeholders to discuss solutions, and we are so grateful to AACIPM for creating these opportunities.”
To watch any or all of the day’s events or download the slides, visit AACIPM’s site.
AACIPM is hosting another symposium on Nov. 12, “Behavioral Health Approaches for People with Chronic Pain,” in collaboration with the American Psychological Association. Details will be posted soon at painmanagementalliance.org/bha.
