Any health condition that causes chronic pain is difficult to handle, but research increasingly shows that certain individuals are physiologically more prone to developing chronic pain conditions of any kind, and that the interconnectedness between some of these conditions may be greater than yet understood. Over the last two decades, “not one study but hundreds of studies” have shown that people with chronic pain have physiological differences in the way their brain processes sensory information, explains Christin Veasley. Veasley is the cofounder and director of the Chronic Pain Research Alliance and advocates for improved care through more research and educational initiatives. She has served on many federal committees and collaborative alliances, has been a presenter at over 30 medical, research, and policy conferences, and is frequently interviewed for print, television, and radio media.
“To me, that’s been one of the most transformative things that has happened over the last couple decades,” says Veasley. “We finally have something definitive to say, ‘I’m not crazy,’ it’s not a weakness or psychological issue—neurologically, people who develop these conditions are not the same as those who don’t.” Therefore, while it may originate in the brain, it’s certainly not “all in their head,” like many patients, especially those assigned female at birth, may have been told at some point.
This research has identified and begun to investigate the interrelationship between pain conditions in different areas of the body as well as other non-pain comorbidities. Overlap is the norm rather than the exception: for example, according to the U.S. Pain Foundation’s 2021 Pediatric Pain Survey, 80% of surveyed children live with three or more confirmed medical diagnoses, including mental health and other non-pain comorbidities. Similarly, 95% of respondents in the U.S. Pain Foundation’s 2022 survey for adults living with pain reported having at least one comorbidity.
Veasley knows that interrelationship well: she first experienced chronic pain following a near-fatal car accident, and developed multiple other pain conditions over the decades. She learned that pain usually involves a trigger, like an illness or an accident, but that someone with a family health background may be more “genetically primed” to develop chronic pain conditions than the average individual.
There have been multiple terms coined to describe this, like “central sensitization syndrome,” but the common denominator is the central nervous system. Just as cancer may present in different ways based on location, these chronic pain conditions may have the same basic mechanism but manifest differently.
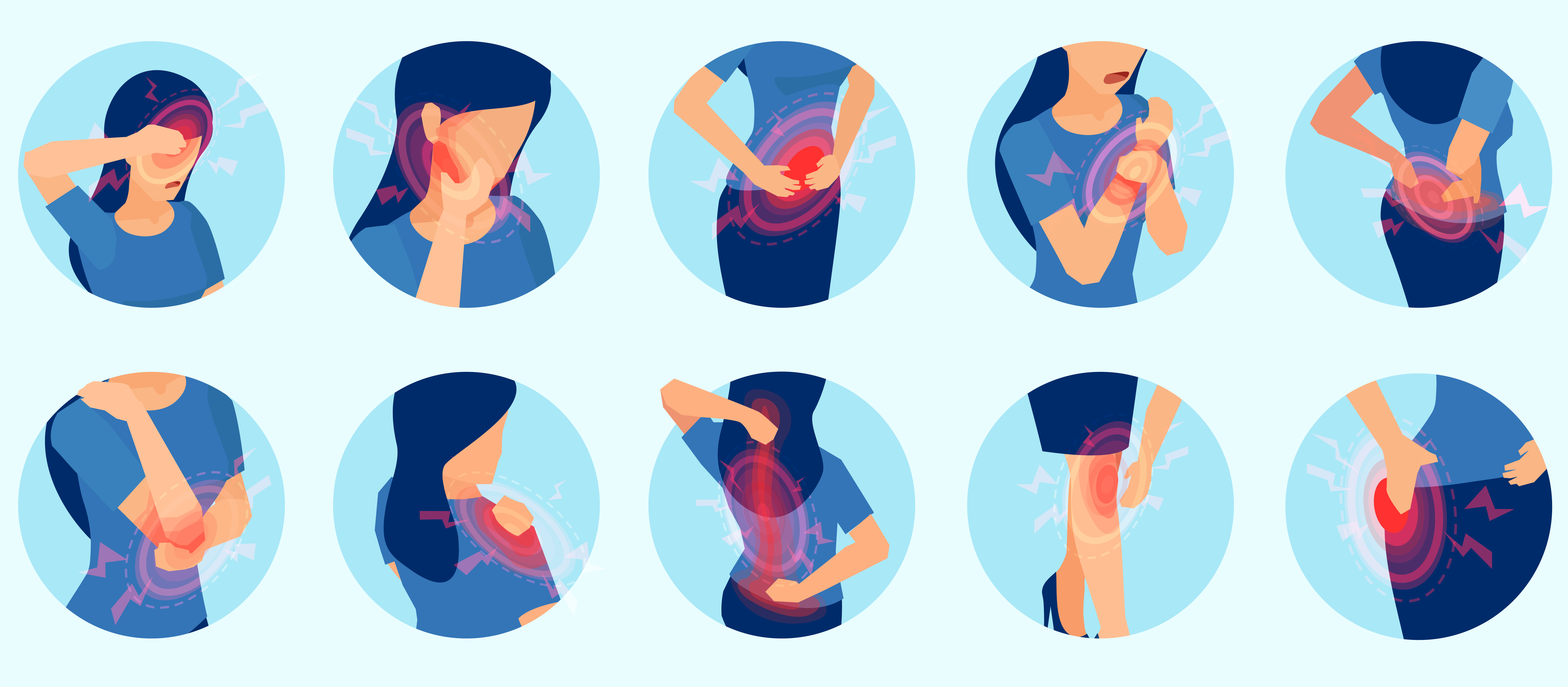
In fact, certain conditions—chronic fatigue syndrome, chronic low back pain, chronic tension headache, endometriosis, fibromyalgia, migraine, interstitial cystitis/painful bladder syndrome, irritable bowel syndrome, temporomandibular disorder and vulvodynia—occur so frequently together that the term “chronic overlapping pain conditions” (COPCs) was coined to identify them.
Downsides of Specialization
It took so long to identify the interrelatedness of these conditions in part due to the increasingly siloed state of American healthcare, where pain conditions are classified by body area or organ. But when each doctor only focuses on their area of specialization, more systemic problems can be missed.
It’s a widespread issue: the U.S. Pain Foundation recently published its findings from a nationwide survey earlier this year that showed only 30% of respondents living with pain feel they are a team with their current health care professionals in managing their pain, and 67% do not feel supported by their providers. Veasley encourages patients to disclose all their health issues to their clinicians, not just the one they are seeking immediate care for or the ones that fall under that clinician’s purview.
But patients can be hesitant to introduce a problem that is “out of scope.” For instance, in the same U.S. Pain survey, 93% of respondents living with fibromyalgia also experience frequent headaches. But 28% of those individuals had not discussed their head pain with their doctor. In an article written by Michele Rice, patient engagement lead for U.S. Pain, for National Migraine and Headache Awareness Month, she compared this conundrum to a car. When her other, more pressing, health problems were an urgent “flat tire,” her headaches were put on a back burner, like a “check engine” light that she was able to ignore—until she couldn’t anymore.
Prevalence, Priorities, and Speaking Out
Unfortunately, modern medicine has only begun to understand the mechanisms behind these pain conditions and what effect genetics may have on their prevalence. One in five Americans have some form of pain, but competition for health care dollars against more fatal or infectious diseases is a major factor holding back investigation into the underpinnings of pain-related diseases. In addition, much of the current research is funded through the NIH’s HEAL Initiative so has been in the specific context of reducing opioid misuse and overdose.
An enormous number of people are affected by chronic pain conditions, but few talk about it publicly. “There are so many reasons we haven’t gotten attention at the federal level over the last many decades, but at the same time, the squeaky wheel gets the grease,” explains Veasley. “If everyone with chronic pain were to do a few key things to raise awareness and to talk with their congressional representatives about it, we could make so much more progress in a shorter period of time.”
“There’s still so much bias attached to chronic pain, like it’s a personal weakness,” adds Veasley. “We’ve gotten to the point where it’s understood that a lot of people have pain conditions, and it’s OK to have, but the moment you acknowledge that you’re impacted by it, that it affects your ability to work or engage in social functions or take care of your children, then there’s still that bias attached that you’re perceived to be less strong than another person who could just overcome and keep right on rolling.”
Significant reforms need to take place in America for doctors to have the time and ability to treat chronic pain in a holistic way, but they all start the same way: by gathering together and speaking out. “Until people appreciate the true societal burden of pain, we’re not going to get the changes we need,” says Veasley. “We’ve long known that pain was highly prevalent, and long known it’s very costly. So why are we not doing more about it as a society?”
