Even the most cautious, careful person will experience hundreds of instances of pain in their lifetime. A stubbed toe. A paper cut. Sore muscles after a strenuous workout. A bad sunburn.
These are all examples of what is known as acute pain, an unpleasant sensation that is the body’s way of signaling some kind of damage. Acute pain tends to be short term and typically is resolvable, but there isn’t a lot of consensus even among health care professionals about the best treatment options or even how to define acute pain.
“It’s eye-opening how little doctors are trained on how to treat pain,” says David Nagel, MD, a physiatrist specializing in pain management for 30 years and author of Needless Suffering; How Society Fails Those With Chronic Pain. “It leads to so much incredible variability on how these issues are handled.” To help better educate and empower patients and industry professionals, Nagel helped author a Pain Management Guide.
Pain defined
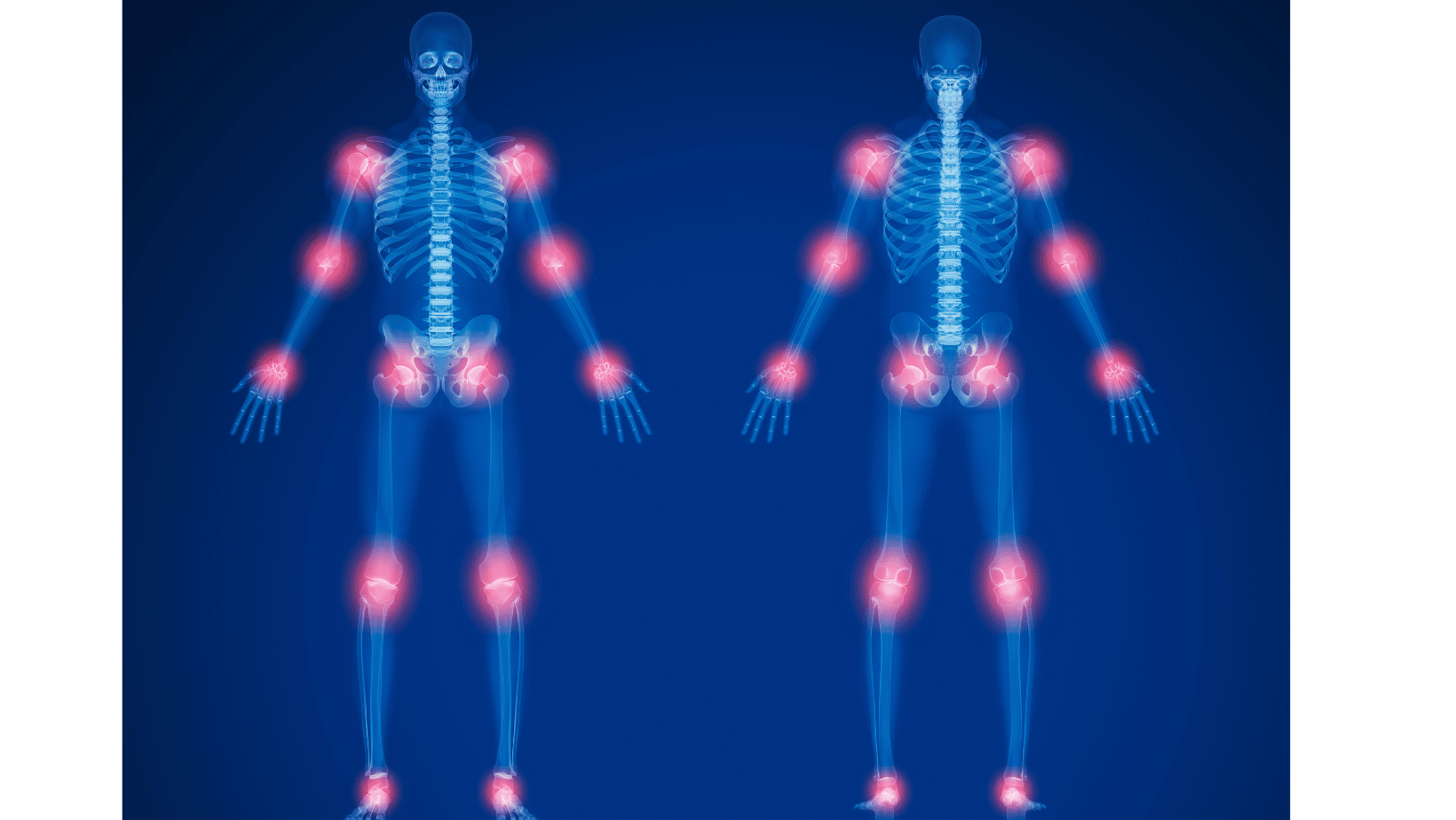
Understanding pain better can help us manage it more efficiently. While pain is a universal human experience, there are many different ways to classify it. In the broadest terms, pain can be divided into nociceptive and neuropathic. The former is what we feel when we touch a hot stove or pull a muscle; it is a response to damage from an outside source. Neuropathic pain, on the other hand, comes from nerve damage or dysfunction.
Most of the time when we experience acute pain, it is nociceptive pain, Nagel says. It persists until the structural damage to the body heals—a cut scabs over, or muscle fibers regenerate. In general, this process tends to take three months or less; if pain persists beyond that point, it may have become neuropathic pain or chronic pain. In those cases, says Nagel, “The pain signal, rather than the structural issue, becomes the problem.”
While it is unknown exactly how often acute pain becomes chronic, Nagel says the industry rule of thumb is around 10% of cases. “The likelihood of any acute pain becoming chronic is relatively small,” he says. “That said, chronic pain usually starts as acute pain.” So it’s worth paying attention to: 50 million adult Americans live with chronic pain, which is “hardly a small number,” Nagel says.
Of course, there are exceptions even to the broad definition of acute pain. Nagel points out that with a disease like osteoarthritis, “that pain is technically acute pain even though it goes on for years and years.” Likewise, re-injuring an old wound can cause acute pain that lasts longer than the standard three months. For these reasons, it’s important to look at all aspects of pain and the circumstances surrounding the person experiencing it when determining the best treatment options. Some other considerations include:
- Point of origin. Nagel deals mostly with orthopedic and neuropathic pain, but there is also visceral pain, which originates internally.
- Severity. If pain is mild to moderate, people typically tend to deal with it on their own, instead of seeing a doctor—unless it doesn’t go away in a reasonable amount of time.
- Consistency. Pain can be constant or intermittent.
- Impact on quality of life. If your ankle only throbs when you drive long distances, it may not present a problem—unless you work as a truck driver. “If pain is not interfering much with your quality of life, most people will be willing to tolerate it longer,” says Nagel.
- Risk to health. A sore arm is probably not going to worry you if you are in otherwise good health and overdid it at the gym the previous day. A shooting pain in the left arm out of the blue, however, is a sign of a possible cardiac event. “If someone thinks their pain is potentially life-threatening, they may get treatment sooner,” Nagel says.
Treatment options
The good news is that in most instances, acute pain can be treated fairly easily at home. Depending on the injury, you can use the RICE model (rest, ice, compression, and elevation) or other appropriate first aid. Nonprescription painkillers are a helpful option as well. “I think there’s no better anti-inflammatory than ibuprofen, and that’s over-the-counter,” says Nagel.
If those measures don’t help, people usually seek out a doctor for professional advice. But again, without much standardization in care, “it’s totally dependent on who you see,” Nagel says. Often, health care providers will call for expensive imaging tests (which Nagel says may not even be necessary), call for prescription painkillers, and send the patient on their way.
Nagel believes there is a better way. One of the most important tenets of pain management, he believes, is taking a holistic approach. “You have to look at the whole person and not just the injury,” he says. “In what setting did the pain occur, how has it been affecting their quality of life, even the psychosocial aspects of the injury.”
There’s good evidence that a negative emotional or social response to an acute injury can promote the development of chronic pain—for instance, if an individual is accused of malingering, or does not receive good support at home or in the workplace in the aftermath of their injury. The best approach from a health outcome perspective, according to Nagel, is to show support for an injured person as more information is gathered.
He also advocates an overall active strategy compared to a passive one. In other words, while doctors used to prescribe bed rest, now it’s more accepted to use rehabilitation techniques for orthopedic pain. “Activity is a lot better than passivity at treating problems,” says Nagel. He recommends those who experience acute pain to implement a brief period of self-care at home, and if that doesn’t seem to be helping, to seek out restorative options. Those he endorses include chiropractic care—”the whole field is way different than it was 10 years ago,” he says—massage therapy, low-level lasers, acupressure and acupuncture, and electrical stimulation devices.
Nagel’s guide, as well as the MyPainPlan resources that can help with acute pain in addition to chronic pain, can be a good go-to for more information on these techniques, so that you can discuss the options with your health care provider. Because of the distinct possibility that acute pain can transition to chronic, taking proactive measures as quickly as possible can make a difference after an acute injury or event.
–by Jill Waldbieser
This campaign was created through support from Vertex Pharmaceuticals and Johnson & Johsnon. U.S. Pain Foundation developed the content without review from sponsors. This information is educational only and should not be used as a substitute for advice from a health care professional.
Subscribe to our newsletter
U.S. Pain Foundation is a 501 (c)(3) nonprofit organization dedicated to serving those who live with conditions that cause chronic pain, as well as their caregivers and care providers. Learn more.
Our Sponsors
U.S. Pain Foundation relies on the generosity of donations and grants. We are especially thankful to our Corporate Council for sustaining our programs and services year-round. Learn more.
Contact Us
U.S. Pain Foundation, Inc.
15 North Main Street, Unit 100
West Hartford, CT 06107
Telephone: 800.910.2462
Email:
contact@uspainfoundation.org
Tax ID number: 26-2703521
All Content Copyright 2021 | All rights reserved. U.S. Pain Foundation is a qualified 501(c)(3) tax-exempt organization. Disclaimer
