 Some of our community members, because of underlying health conditions, fall into the higher-risk category for developing serious coronavirus or COVID-19. In addition, as the illness spreads, so does misinformation.
Some of our community members, because of underlying health conditions, fall into the higher-risk category for developing serious coronavirus or COVID-19. In addition, as the illness spreads, so does misinformation.
With that in mind, we wanted to highlight some current facts about COVID-19, including:
- How the illness spreads
- Risk factors for severe illness
- Precautions and preventing spread
- Severity of disease
- Symptoms and when to seek care
- Treatment
- More tips and resources
Please note that as the situation evolves, information may change or be updated. U.S. Pain Foundation is providing this educational overview as a courtesy; if you have specific questions, please contact your health care provider.
How the illness spreads
Experts believe COVID-19 spreads mainly from person-to-person contact. It is possible—but less likely—that you become infected by touching a surface or object that has the virus on it and then touching your own mouth, nose, or eyes.[1]
According to the Centers for Disease Control and Prevention (CDC), person-to-person contact occurs:
- Between people who are in close contact with one another (close contact is defined as six feet or less)
- Through respiratory droplets produced when an infected person coughs or sneezes. These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs.[2]
It’s important to note that the disease may be spread before an individual begins showing symptoms.[3] That also makes it important to be mindful of the incubation period, or the time from infection to start of symptoms. According to a recent study from Johns Hopkins, the median incubation period for COVID-19 is estimated to be approximately five days.[4] (As with all COVID-19-related research, which is in early stages, this number may change over time.)
Risk factors for severe illness
By now, most of us have heard that possible risk factors for progressing to severe illness may include, but are not limited to, older age and/or underlying chronic medical conditions. Most reports only give three examples—heart disease, lung disease and diabetes.
Here is a more detailed list, according to the CDC[5]:
- lung disease
- cancer
- heart failure
- cerebrovascular disease
- renal disease
- liver disease
- diabetes
- immunocompromising conditions
- pregnancy
It is recommended that individuals with risk factors take extra precautions to avoid contracting the illness.
Precautions and preventing spread
For all individuals, practicing good hygiene—avoiding contact with the ill or individuals who may have been in contact with the ill; washing your hands sufficiently; avoiding touching your face; and cleaning common surfaces—is always smart.
It is important to note, however, that good hygiene practices are not foolproof. This is especially true given that the disease is believed to spread through airborne droplets and that individuals may be contagious while asymptomatic.
With that in mind, the most effective way you can prevent the spread of disease is to limit person-to-person contact.
The CDC lists the following special precautions for higher-risk individuals:
- Stocking up on supplies, like food and medication. (Note this is not necessarily because either will not be available, but instead to help limit your need to go outside. Also, insurance coverage may not always allow for stocking up on medication. But you can try asking for an exception.)
- Taking everyday precautions to keep space between yourself and others.
- When out in public, keeping away from others who are sick, limiting close contact and washing your hands often.
- Avoiding crowds as much as possible.
- Avoiding cruise travel and non-essential air travel.
- During a COVID-19 outbreak in your community, staying home as much as possible to further reduce your risk of being exposed.[6]
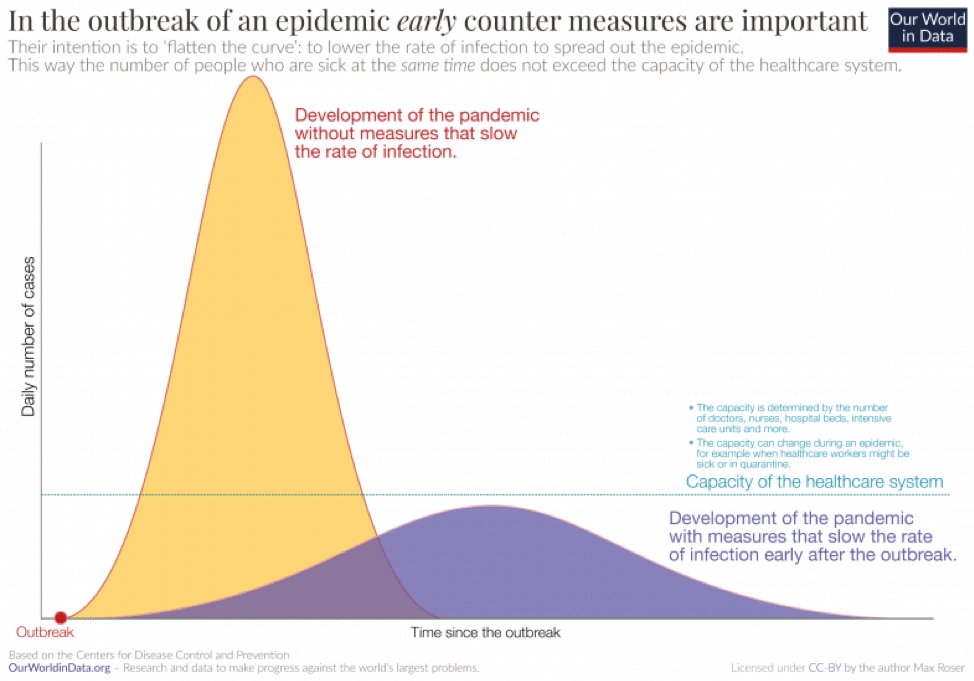
A number of experts are using the term “flatten the curve” to describe how early precautionary steps—even though they may seem excessive—are vital to controlling a steep increase in disease spread.[8]
Avoiding this steep increase in disease spread is helpful in many ways, including ensuring that the health care system is not inundated with severe cases beyond its capacity to treat them. This chart, which is based on data from the CDC, depicts the “flatten the curve” concept.
Severity of disease
Early research, published in the Journal of the American Medical Association (JAMA), seems to indicate the virus may be more serious than the flu.[9]
According to this study, which analyzed more than 44,000 confirmed cases in China :
- 81 percent of patients had mild illness
- 14 percent had severe illness
- 5 percent had critical illness
It’s important to note that these numbers are very preliminary, and will likely change over time. In particular, it’s possible the percentage of mild cases is higher, as they are less likely to need treatment and, therefore, to be officially reported.
Symptoms and when to see care
As indicated by the JAMA study, most cases of COVID-19 will be mild.[10] However, it is good to be mindful of what symptoms to look out for, especially to help differentiate them from the common flu or a cold.
Below is an excellent chart about the likelihood of specific symptoms of COVID-19, based on information from the World Health Organization.
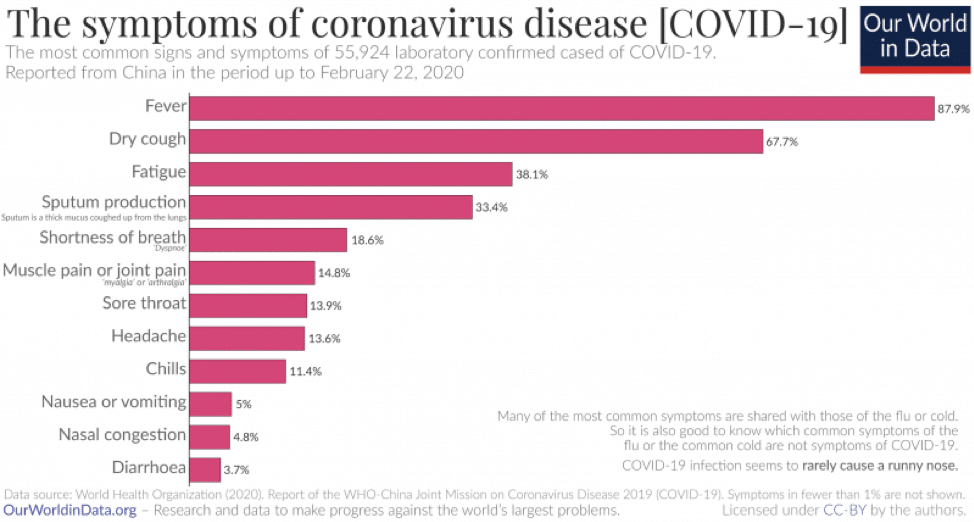
If you feel like you are developing symptoms that characterize COVID-19, the CDC recommends you call your doctor for medical advice and stay home, except if you need to get medical care.[11] Remember, again, that most cases are mild and will resolve on their own.[12]
If you develop emergency warning signs for serious illness from COVID-19, you should get medical attention immediately. According to the CDC, in adults, emergency warning signs* include:
- Difficulty breathing or shortness of breath
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Bluish lips or face
*This list is not all inclusive. Please consult your medical provider for any other symptoms that are severe or concerning.
Treatment
Specific treatment for COVID-19 is not currently available. Clinical management includes “prompt implementation of recommended infection prevention and control measures and supportive management of complications.”[14]
An avalanche of research is being done on a possible vaccine. But even if a vaccine is found, it will take at least several months, if not much longer, before it is widely available.[15]
This is why it is vitally important to limit spread, especially for high-risk populations.
More tips and resources
Being a pain warrior means you are incredibly resilient, and know what it takes to be strong in challenging situations. But because of underlying chronic health conditions, some pain warriors may fall into a high-risk category for developing serious COVID-19.
Out of abundance of caution, we encourage you to:
- Educate yourself with information directly from reliable sources, like government agencies and academic medical centers
- Contact your health care provider if you have concerns or symptoms
- Take extra measures to prevent the spread of disease
Your safety is our utmost concern. It is difficult to know what measures may eventually be considered overreacting—or underreacting. But at this early stage in the situation, which continues to evolve, we believe it is best to err on the side of caution.
For more information on COVID-19, we recommend visiting the following resources:
- The Centers for Disease Control and Prevention
- The World Health Organization
- Johns Hopkins Hospital
- Massachusetts General Hospital
Finally: if you are feeling extra stressed or anxious about your health or the current situation in general, we strongly encourage you to jump on one of our free support calls, which take place four times a month on Thursdays, and once a month on Saturday.
Sources
[1] https://www.cdc.gov/coronavirus/2019-ncov/about/transmission.html
[2] https://www.cdc.gov/coronavirus/2019-ncov/about/transmission.html
[3] https://www.health.harvard.edu/diseases-and-conditions/coronavirus-resource-center
[4] https://hub.jhu.edu/2020/03/09/coronavirus-incubation-period/
[5] https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html
[6] https://www.cdc.gov/coronavirus/2019-ncov/specific-groups/high-risk-complications.html
[7] https://www.cdc.gov/coronavirus/2019-ncov/about/steps-when-sick.html
[8] https://www.statnews.com/2020/03/11/flattening-curve-coronavirus/
[9] https://jamanetwork.com/journals/jama/fullarticle/2762130
[10] https://jamanetwork.com/journals/jama/fullarticle/2762130
[11] https://www.cdc.gov/coronavirus/2019-ncov/about/steps-when-sick.html
[12] https://jamanetwork.com/journals/jama/fullarticle/2762130
[13] https://www.cdc.gov/coronavirus/2019-ncov/about/symptoms.html
[14] https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html
[15]https://externalmediasite.partners.org/Mediasite/Play/45a9a74f18ec45deb338e00ac4cf4e281d?fbclid=IwAR1ThtC7jtEPJ8DmDpsUFjBZ8RfcbcmWaVPDGypp2L7tTYj_AT2iBLgh2FU
