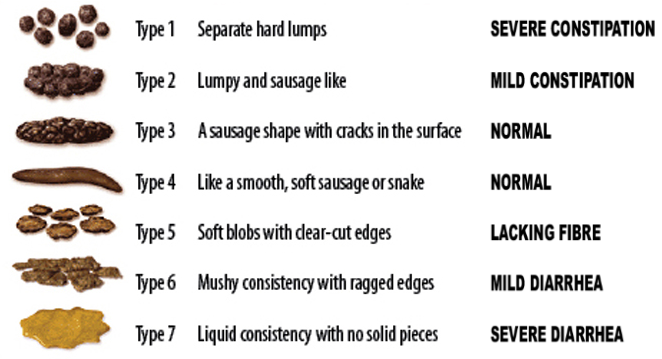
One common cause of chronic pain that people can be hesitant to talk about is constipation. Every person’s body is different, and the frequency of healthy bowel movements can vary widely: it can be healthy for some people to go multiple times a day, others less frequently. However, three or fewer bowel movements in a week is considered to be constipation. A tool called the Bristol Stool Scale (see image below) can help to determine whether constipation is an issue based on the visual appearance of bowel movements.
Typical causes of constipation
Constipation has a wide range of possible causes. Although most people experience this problem at some point in their life — about 16% of adults in the US are constipated at any given time[1] — it usually resolves relatively quickly and without the need for medical intervention. Unfortunately, sometimes constipation can be the result of simply changing your diet, daily routine, or just from stress.
There are a wide range of medical conditions that can cause constipation, and many widely-used medications list constipation as a possible side effect. Patients taking opiates must pay special attention to this possible consequence as it can cause changes to the stomach.
Everyday options to prevent constipation

There are a wide range of fiber-rich foods that can help ease this condition, including fruits like apples, bananas, prunes, pears, raspberries, and vegetables like string beans, broccoli, spinach, kale, squash, lentils, peas, and beans as well as nuts and food with bran in it. But stay aware of how much: more than 25-30 grams of fiber a day can cause bloating.

Stay active to stay active

Besides diet and hydration, physical activity is the greatest lifestyle factor affecting constipation. Moving around keeps the muscles in the abdomen working, including the ones that move the stool through the digestive system. Getting a healthy amount of exercise doesn’t just make you fit, it helps keep you regular too. Patients should also be encouraged to go to the toilet as soon as they feel the urge if at all possible.
Medical causes of constipation
There are a variety of medical conditions that have constipation as a side effect. These include (but are not limited to):
- Bowel or intestinal obstruction
- Structural defects in the digestive tract
- Endometriosis
- Fibromyalgia
- Diabetes
- Inflammatory bowel disease (IBD) (including ulcerative colitis and Crohn’s disease)
- Irritable bowel syndrome (IBS) and lazy bowel syndrome
- Liver disorders (including cancer, cirrhosis, and hepatitis)
- Multiple Sclerosis (MS)
- Colorectal cancer
- Hypothyroidism
- Pelvic floor disorders
- Peritonitis
- UTIs (Urinary tract infections)
- Celiac disease
- Lupus

Constipation is also a significant side effect of some medications. These include:
- Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen
- Antidepressants, including selective serotonin reuptake inhibitors (SSRIs) or tricyclic antidepressants
- Antacids
- Iron pills
- Allergy medications like antihistamines
- Certain blood pressure medications, including calcium channel blockers and beta-blockers
- Anticonvulsant/seizure medication
- Anti-nausea medications
- Opiate pain medications
Opiate Medication and Constipation
Opiates relieve pain by activating receptors in the brain, but these receptors are also found in the gastrointestinal (GI) tract. Because of this, the use of opioid medications very often causes GI problems. While typical constipation can be caused and solved by lifestyle factors, opioid-induced constipation (OIC) results from the physiological changes that opiate medications cause in the body. This means the issue will not improve on its own over time as with some other side effects.
OIC may present immediately after starting the medication or develop gradually over time, and is more likely to develop the longer the treatment is continued.[1] This makes the management of constipation a crucial pain management issue to address from the start.
[1] https://www.ncbi.nlm.nih.gov/books/NBK493184/
Preventing Opioid-Induced Constipation
Patients beginning narcotic medications should know about the need to hydrate, stay active, eat a high fiber diet and avoid other medications that may cause constipation. Patients should also begin taking a laxative at the same time that opiate therapy is begun.
Doctors will often recommend the use of a stimulant laxative like bisacodyl, sodium bicarbonate with potassium bitartrate, senna, or castor oil. These work by increasing peristalsis, the movement of the muscles in your digestive tract. This is sometimes combined with stool softeners, which can help prevent constipation but are less effective for patients already suffering from OIC. Another option is an osmotic laxative (Miralax, lactulose, and milk of magnesia), which helps pull water into the intestine. These are considered safer for long-term use than stimulant laxatives. Bulk-forming laxatives like psyllium, Metamucil, Citrucel, or Fibercon are the one type of laxative that patients with OIC should avoid. These cause an increase in the bulk of the stool, which, accompanied by the lack of peristaltic movement caused by OIC, can actually exacerbate pain or even cause a bowel obstruction.
If these options don’t solve the problem, there are a variety of prescription medications available to try. But whichever treatment your doctor suggests, it’s important to stay in close communication with your medical team about any GI problems you may experience so they can be treated before they grow into bigger issues. And if you see blood in your stool or are running a fever in addition to being constipated, call a doctor immediately.
Unfortunately, once OIC develops it can be very difficult to bring the GI tract back to its original state, so it’s something that doctors should address at the outset when prescribing opiates. Anticipating the issue before symptoms appear removes a significant barrier to the effective management of chronic pain
What to Remember when it comes to constipation
Almost every person has experienced constipation at some point, but for individuals living with chronic pain, it can become a significant medical issue. Despite how common an experience it is, it’s natural to be shy about talking about constipation and other GI issues. But anyone with chronic pain who experiences constipation should contact their doctor to see what options there are to treat it. It’s nothing they haven’t heard before! So chronic pain patients shouldn’t hesitate to communicate their constipation-related issues with their medical team, and always keep them informed before trying anything new.