By Stephani Sutherland
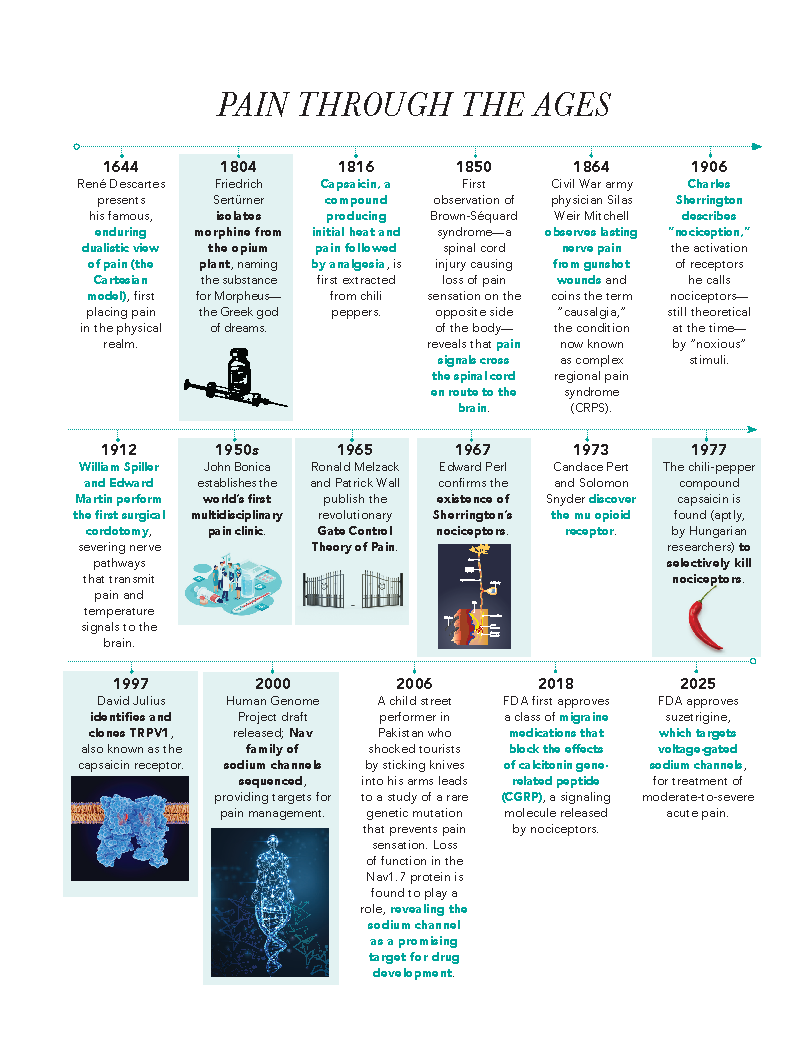
Humans have always lived with pain—and history suggests we’ve always tried to alleviate it. The study, understanding, and treatment of pain have evolved significantly throughout the ages.
For decades, Allan Basbaum, PhD, has occupied a front-row seat to formative research advancements. Basbaum—a neuroscientist and chair of the Department of Anatomy at the University of California, San Francisco (UCSF)—has made substantial contributions to pain research, in addition to working with and training other leading pain scientists.
Currently, his lab at UCSF investigates the ways that tissue and nerve damage can lead to changes in the nervous system that produce persistent pain—continuing to work at the cutting edge of pain science.
Early 20th century: Sensory activation and nerve pathways
Before Basbaum’s time, around the start of the 20th century, the physician Charles Sherrington first described the process of nociception—the activation of sensory neurons throughout the body, which he called nociceptors, by “noxious” stimuli that ultimately produce pain. By that time, morphine was already the gold standard for pain relief, and battlefield medicine during the U.S. Civil War had taught doctors much about pain.
Early researchers had some understanding that pain was a complex human experience entangling not just sensation but thought and emotion. And it became clear, particularly in the wake of more wars that left veterans experiencing chronic pain, that pain didn’t always disappear after an injury healed.
In the 1950s, a larger-than-life character named John Bonica—a World War II Army anesthesiologist and former professional wrestler—established the nation’s first multidisciplinary pain clinic, in Washington state. His early vision laid the foundation for the biopsychosocial model of pain, which guides best treatment practices today. He later convened a symposium on pain in 1973 that soon culminated in the founding of the International Association for the Study of Pain (IASP), garnering recognition for pain research.
But despite these gains, the dualistic Cartesian model of pain established by René Descartes in 1644—separating the physical body from the immaterial mind and arguing that pain lacks a psychological component—still held sway. Centuries later, pain was widely understood as a signal that simply traveled from the body to the brain, just as telephone signals once zipped along wires.
“Historically, there used to be the notion of a pain pathway,” says Basbaum. “You have an injury, and the pain pathway goes to the brain. You want to get rid of it, poof—you just cut it.”
For years, that was accomplished through a surgical procedure called a cordotomy, first performed in 1912 to sever those nerve pathways. The surgery is rarely performed today; although it works for a while, the pain generally returns, sometimes worse than before.
Pain processing, Basbaum says, “is not a telephone wire system. It’s much more complex.”
Mid-century: Fresh perspective on pain’s journey to the brain
That complexity was revealed in the Gate Control Theory of Pain—a seismic development for the field, developed in 1965 by psychologist Ronald Melzack and neuroscientist Patrick Wall.
Basbaum later worked with both men. His serendipitous entry to the field of pain research was a summer job working for Melzack as an undergraduate at McGill University in Montreal, just two years after the gate control theory was introduced—an opportunity that led Basbaum to turn down a coveted job at Expo 67, Canada’s centennial world’s fair. Several years later, he also worked with Wall in London, who was at the time the world’s preeminent pain scientist, Basbaum says.
Melzack and Wall postulated that small, pain-provoking nociceptive neurons and larger sensory neurons reacting to innocuous stimuli, such as pressure or vibration, somehow compete to communicate with spinal “projection” neurons. That interaction opens or closes a neurological “gate” in the spinal cord, regulating which signals are transmitted to the brain.
For instance, Basbaum describes, why do you shake or rub your hand after burning it? “You stimulate it more; that seems crazy.” But activating the larger sensory nerve fibers helps inhibit the pain-responsive nociceptors at the spinal cord. “That’s the closing of the gate,” he explains.
The theory also describes the ability of the brain itself to assess those inputs and regulate the gate in some cases, he says—consider a football player not immediately realizing they’ve broken their leg due to a phenomenon called stress-induced analgesia.
Modern times: Temperature receptors and targeted treatments
In the years following, researchers made incredible discoveries about pain in the brain. In the 1970s, neuroscientist Edward Perl famously identified nociceptors as a distinct class of sensory neurons, proving Sherrington’s theory from decades before.
He also identified spinal neurons that were specialized for the transmission of pain-provoking messages, indicating distinct pain-related nerve pathways that could be targeted.
The 1970s also saw the discovery of the mu opioid receptor, a protein in the central and peripheral nervous systems, and endogenous opioids, the neurotransmitters that interact with those receptors. Basbaum’s early work helped identify how opioids affect neural circuits in the brain and spinal cord to alleviate pain.
By the end of the 20th century, researchers had adopted a strategy to develop new therapeutic agents for pain: to target—and ideally silence—nociceptors, the sensory neurons that initiate painful signals using specialized receptor proteins.
Rapidly developing technology allowed researchers to sequence the genes for these proteins, and to study the effects of removing or modifying them in transgenic, or genetically modified, mice. Building on investigations in people and animals from recent decades, researchers raced to identify and genetically sequence the proteins that sensed hot and cold, acid, pressure, inflammatory substances—and a substance called capsaicin.
Capsaicin, the compound that makes chili peppers hot, was isolated early in the 19th century for its analgesic properties. Later, researchers discovered that it both selectively activates nociceptors—allowing them to study the neurons in different ways—and selectively kills nociceptors. As the molecular biology revolution heated up in the 1990s, so did the hunt for the distinct capsaicin receptor.
Ultimately, that discovery was made by UCSF biochemist and physiologist David Julius, who identified and cloned the TRPV1 receptor in 1997. Even more impactful: The discovery that TRPV1 also acts as a molecular heat sensor. Julius and his team went on to identify other members of the TRP gene family that respond to temperatures ranging from icy cold to burning hot, and to plant chemicals such as menthol. Through three decades of collaborating on various projects at UCSF, Basbaum and Julius have co-authored more than 20 research papers, including one outlining the capsaicin receptor’s heat interactions.
In 2021, Julius received the Nobel Prize in Physiology or Medicine for his work on the TRP family of sensory proteins. He shared the prize with Ardem Patapoutian, a neuroscientist and molecular biologist at the Scripps Research Institute in San Diego who discovered the Piezo proteins, which sense mechanical forces such as touch or pressure.
Many of the proteins found in nociceptors have now become “targets” for development of new drugs.
“We understand a lot about how pain is generated—the pathways, the circuits, the molecules—and we have lots of targets,” Basbaum explains. “So that should provide the basis for generating novel therapies.”
But turning breakthroughs into treatments takes time.